RJ is a 13-year-old male, typical in most ways. He attends school and likes to share YouTube videos with his friends. He has never had any serious health problems aside from some ear infections as a young child. After a recent sleepover at a friend’s birthday, RJ developed flu-like symptoms including a cough, fever, and muscle aches. Later, he found it more difficult to breathe and lost his sense of taste. After his parents became concerned, he arrived at the emergency department (ED) of the local children’s hospital. On admission, he had fatigue, low oxygen levels, measured 5 feet 6 inches tall, and weighed 219 pounds. RJ tested positive for COVID-19 and began receiving supportive care. After 8 days of treatment in the hospital, his breathing improved and he was able to return home. Only a slight cough remained.
– A Case of COVID-19
What’s The Story
Real Life Consequences
Obesity has become a public health concern within the human population. However, conversations regarding its overall impact on health and beauty standards have more recently been called into question. Although the medical definition of obesity is well framed, popular media has often combined and confused the idea of healthy weight with ever-changing cultural ideals of body standards and attractiveness.
Let’s Set the Record Straight

Bodies come in an enormous range of shapes, sizes, colors, and variations. This is a good thing! Genetic diversity is the backbone of a healthy population in any animal species and humans are no exception. This ensures enough variation in our genes to keep us able to respond to our ever-changing world and slow the spread of genetic defects. So why all the concern? Just as with extremes in environment, extremes in body composition are not beneficial to health.
Health and Body Size
When someone becomes too thin, or emaciated, a person is at risk of developing problems in various body systems. Poor immune function, brittle bones, and an abnormal heartbeat are just a few of these issues. If someone becomes too overweight, or obese, people are yet again at risk of body system failure but for different reasons. A weak immune system, joint stress, and cardiac strain to name some corresponding problems. In children, these effects are especially concerning because this wear and tear begins at a younger age, exposing them to potential health problems sooner in their lives. But what does this have to do with COVID?
Obesity as a COVID-19 Risk Factor
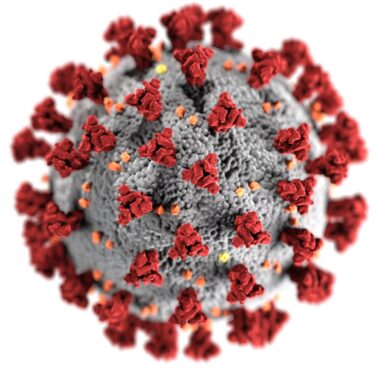
Since the emergence of SARS-CoV-2 (the virus that causes COVID-19 illness), more evidence has shown that adults living with morbid obesity have a higher risk of hospitalization, intensive care unit (ICU) stay and death from COVID-19. On the whole, children are at less risk of severe COVID illness than adults. Sometimes they may not show symptoms at all. New data, however, show that obese children are more likely than their average weight peers to have more serious illness.
Skeptical? I certainly was, and skepticism makes me incredibly curious. So, I began to follow my pediatric COVID-positive patients closely and the data tells an incredible story.
Research Results
The Patients Studied
Over several months I gathered data from patients admitted to the hospital. It appeared true that sometimes when kids test positive for COVID, they may not get seriously ill. In fact, about 24% percent of all studied patients did not show any COVID symptoms even after testing positive. These patients were admitted to the hospital for other reasons. They were found to be SARS-CoV-2 positive only because the hospital automatically tests each patient admitted during the pandemic. We call this an incidental finding.
Surprising Results
Interestingly, 100% of the children over 2 years old with severe COVID-19 had a health condition that made them more vulnerable to serious illness. What health condition appeared to be behind most of the admissions? Look no further than morbid obesity. It was clear that 87.5% of the patients with serious symptoms were considered obese. This is significant, especially considering that most of these children did not have other known health conditions. Of the patients who were not obese with serious symptoms, all had underlying medical problems which increased severe disease risk.
See Talk Nerdy To Me for an informational table
Conclusions
Further Questions
It would appear from my research that there is a strong link between obesity and serious COVID-19 illness among children. While the numbers are undeniable, it should be noted that my study has limitations. A larger study may reveal more information about different types of patients who have risks for having severe disease. For example, it is no secret that folks who are disadvantaged are at increased risk for health-related problems as they age. This means that it’s possible disadvantaged children may be more at risk for healthcare problems and be obese. However, the two things may not necessarily be related. This is called correlation bias. The best way to examine the truth of the data is to do more studies using scientific evaluation to eliminate sources of bias.
Final Thoughts
With all this in mind, it is my opinion that no matter the person, the body type, nor age: diet and exercise are the foundation of good health. I cannot say this enough. Diet and exercise should be the cornerstone of anyone’s self-care, healthcare, and welfare. As a pharmacist I often encounter patients who are looking for the next miracle cure or quick fix. No medication that I can provide will replace the health benefits of eating with nutrition in mind. No prescription I fill will provide the long-term benefit of daily exercise on heart health, metabolic health, and mental health. My goal with this article is to raise awareness about the disease progression of COVID-19 in the pediatric population and to encourage further investigation into the role of obesity in this disease.
Talk Nerdy To Me (Details for Professionals and Curious Minds)
Introduction
The SARS-CoV-2 virus has impacted the lives of every person on the planet over the course of the pandemic. As the virus has spread, data and discovery have made living with this novel contagion more feasible. Of particular interest has been evolving data surround which patient populations are most impacted by viral infection. The aim of the research in this article was to observe disease progression among the pediatric population.
Methods
Deidentified data from a tertiary-care pediatric hospital was collected over 5 months in 2021. By this time, the hospital had developed protocols for admission, testing, and treatment for COVID-19. The total COVID positive population was comprised of 25 patients, male and female, of ages ranging from 1 month to 19 years. The standard used for making a determination of obesity is the same used by the CDC (centers for disease control) and is defined as a body mass index (BMI) at the 95th percentile or greater for age, height, and weight. It should be noted that BMI is not applicable for children under 2 years of age and are therefore excluded from obesity related analysis.
Results
Of the 25 COVID positive patients, 21 were greater than 2 years of age and eligible for further analysis. Among these 21 patients: 1 was underweight, 4 were average weight, 1 was overweight, and 15 were obese.
The 21 patients greater than 2 years of age were further stratified. 16 children presented with severe disease and 5 were incidentally positive. Among the incidentally positive patients, the reasons for hospital admission were medical/surgical. Of interest the only obese patient in the incidentally positive group received a complete vaccine series prior to receiving a positive COVID-19 test result.
For the 16 children with severe disease, 14 were obese and 2 were average weight per CDC metrics. Of the 2 patients without obesity, both presented with relevant comorbidities. 1 patient had an underlying autoimmune condition (definitive diagnosis was in progress at time of discharge) and 1 patient had chronic respiratory failure. Within the 14 remaining obese patients, 4 had relevant comorbidities (type 1 diabetes, asthma, chronic respiratory disease, and acute myelogenous lymphoma) and 1 had received a complete vaccine series prior to hospital admission.
Covid-19 Positive Patients Over 2 Years of Age
| Underweight | Average & Overweight | Obese | |
| Total Patients [21] | 4.8% [1] | 23.8% [5] | 71.4% [15] |
| Serious Illness [16] | 0 | 12.5% [2] | 87.5% [14] |
| Serious Illness with Other High-Risk Conditions* [6] | 0 | 33.3% [2] | 66.7% [4] |
| Incidentally Positive [5] | 20% [1] | 60% [3] | 20% [1] |
Discussion
An interesting finding from this pediatric study was the apparent correlation between severe disease and underlying health conditions. Furthermore, the underlying health condition that appeared to be the greatest predictor of disease severity was obesity. Based on available data, adults appear to share this correlation. In this population it has been noted that obesity impairs optimal immune and lung function. Both are vital to overcoming the symptoms of COVID infection and recovering from the illness. It is possible that these findings remain true within the pediatric population. However, the mechanisms for this relationship are beyond the scope of this study.
The study has several limitations which were discussed previously but will go into further depth here. This was a small, single center, observational study of an unknown beta (power) and no confounders were controlled for. With a control group, it would have been interesting to compare the demographics of the COVID + population with the demographics of the general admission population over the same timeframe. A large study with a more diverse patient pool and multivariate analysis is needed to validate these preliminary results and provide any substation to causation vs correlation claims.
References
- Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, Francois F, Stachel A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin Infect Dis. 2020 Jul 28;71(15):896-897. doi: 10.1093/cid/ciaa415. PMID: 32271368; PMCID: PMC7184372.
- Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, Armistead I, Kawasaki B, Meek J, Yousey-Hindes K, Anderson EJ, Openo KP, Weigel A, Ryan P, Monroe ML, Fox K, Kim S, Lynfield R, Bye E, Shrum Davis S, Smelser C, Barney G, Spina NL, Bennett NM, Felsen CB, Billing LM, Shiltz J, Sutton M, West N, Talbot HK, Schaffner W, Risk I, Price A, Brammer L, Fry AM, Hall AJ, Langley GE, Garg S; COVID-NET Surveillance Team. Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 – COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020 Aug 14;69(32):1081-1088. doi: 10.15585/mmwr.mm6932e3. PMID: 32790664; PMCID: PMC7440125.
- Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, Banker SL, Giordano M, Manice CS, Diamond R, Sewell TB, Schweickert AJ, Babineau JR, Carter RC, Fenster DB, Orange JS, McCann TA, Kernie SG, Saiman L; Columbia Pediatric COVID-19 Management Group. Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020 Oct 1;174(10):e202430. doi: 10.1001/jamapediatrics.2020.2430. Epub 2020 Oct 5. Erratum in: JAMA Pediatr. 2021 Jun 21;:null. PMID: 32492092; PMCID: PMC7270880.
- McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020;8:231. Published 2020 Jun 18. doi:10.3389/fpubh.2020.00231
- Kompaniyets L, Goodman AB, Belay B, et al. Body Mass Index and Risk for COVID-19-Related Hospitalization, Intensive Care Unit Admission, Invasive Mechanical Ventilation, and Death – United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355-361. Published 2021 Mar 12. doi:10.15585/mmwr.mm7010e4
For more information or access to the raw data analyzed in these findings, please feel free to contact us.

Coming from a non-medical background, it’s great to have access to scientific information that’s easy to absorb. Insightful and thought provoking – looking forward to more!
Thanks for taking the time to comment. I’m glad that you find the information relatable. More to come 🙂